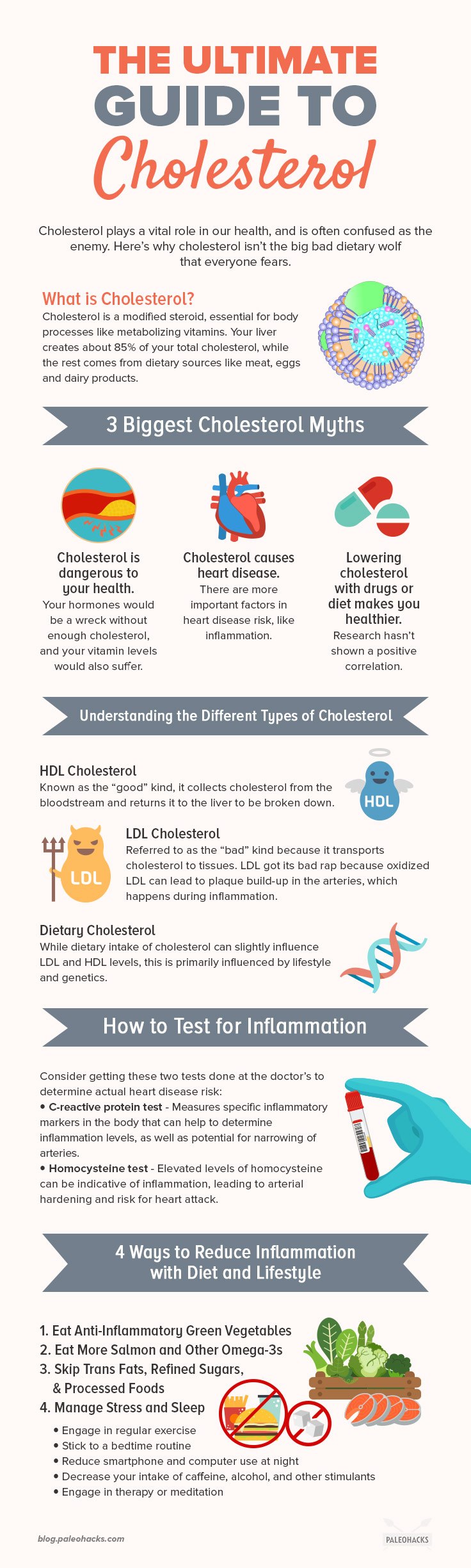
Cholesterol plays a vital role in our health, and is often confused as the enemy. Here’s how cholesterol works and what really causes heart disease.
Recent research has shown that cholesterol isn’t the big bad dietary wolf that everyone fears. In fact, there’s something worse than cholesterol that we should all be mindful of – and most of us eat it every single day.
What Is Cholesterol?
Cholesterol is a sterol, or modified steroid, that is an essential structural component of cell membranes. It is necessary for making sure that membranes are permeable so that fluids and fatty compounds can properly be transported into the blood plasma. (1)
Love turmeric recipes?
Add power-packed anti-inflammatories to every meal with these FREE turmeric recipes!
Cholesterol mainly builds and maintains cell membranes, but it’s also responsible for: (2)
- Producing reproductive and stress hormones
- Creating bile
- Converting sun exposure to vitamin D
- Metabolizing fat-soluble vitamins (A, D, E, K)
- Insulating nerve fibers
Cholesterol is so necessary for these critical body processes that our bodies make 85 percent of it. That’s right – contrary to popular beliefs, cholesterol isn’t a dietary opponent – it’s a critical element of wellness that the body creates. Even if you don’t eat a speck of cholesterol, you’ll have a significant amount in your body because you need it to survive. [tweet_quote]Contrary to popular beliefs, cholesterol isn’t a dietary opponent – it’s a critical element of wellness that the body creates.[/tweet_quote]
The liver produces approximately 800 to 1,000 milligrams of cholesterol per day. (3) The rest of it, about 15 to 20 percent, comes from dietary sources like beef, pork, chicken, fish, shellfish, egg yolks, and dairy products (like milk and cheese).
The cholesterol that we eat isn’t as efficiently put to use as the cholesterol produced by the liver. When what we eat does raise our levels, the liver produces less. So dietary cholesterol has little effect on the actual circulating levels of cholesterol – the ones that get blamed for heart disease risk.
This is where people start to get confused, because many medical professionals have implicated cholesterol in heart disease problems for decades. So let’s dig into the most common cholesterol myths.
3 Biggest Cholesterol Myths

While heart disease is a real health problem, cholesterol isn’t necessarily to blame. Let’s correct these myths, and explore the real culprits in heart disease risk and cardiovascular problems.
1. Cholesterol is dangerous to your health
As discussed above, cholesterol is essential for wellness. Your hormones would be a wreck without enough cholesterol. Your fat-soluble vitamin levels would be insufficient. Your cells would also be starved of proper nutrients and fluid levels.
The general culture talks about cholesterol as if it’s a fat-food monster that clogs your arteries and tries to kill you. Which brings us to:
2. Cholesterol causes heart disease
Cholesterol does not cause heart disease. There are too many factors in heart disease risk to blame one thing, and cholesterol has taken the blame long enough. In the age of low-cholesterol diets, heart disease has only risen, not dropped. Heart disease now accounts for one in every three deaths, up from one in every four. (4)
3. Lowering cholesterol with drugs or diet makes you healthier
Again, we’ve only seen a rise in heart disease deaths since low-cholesterol diets and cholesterol-fighting medication have become popular. Recent research even shows that older folks with higher levels of cholesterol live as long or longer than those with low levels. (5) So, if cholesterol is the great killer that we’ve believed it to be, then why isn’t research agreeing?
Understanding the Different Types of Cholesterol
There are two kinds of cholesterol: the “good” (HDL) and “bad” cholesterol (LDL). In reality, there isn’t anything inherently good or bad about either.
HDL cholesterol, or the “good” kind, is short for “high-density lipoprotein.” It collects cholesterol from the bloodstream and returns it to the liver to be broken down. It got a reputation for being good by sending cholesterol away, but keep in mind that it’s the liver that synthesizes this cholesterol in this first place – so it can’t be all bad.
LDL cholesterol, which stands for “low-density lipoprotein,” is referred to as the “bad” kind because it transports cholesterol to tissues. However, remember that cholesterol is required for hormones and numerous other body processes, and the only way that these can happen is if cells have access to it.
While dietary intake of cholesterol can slightly influence LDL and HDL levels, this is primarily influenced by lifestyle and genetics. But cholesterol isn’t the marker that should be associated with heart disease. In fact, there are several markers that are legitimately more tied to heart disease risk than cholesterol, and the one thing they all have in common is inflammation.
Inflammatory Markers Are the New “Bad” Cholesterol
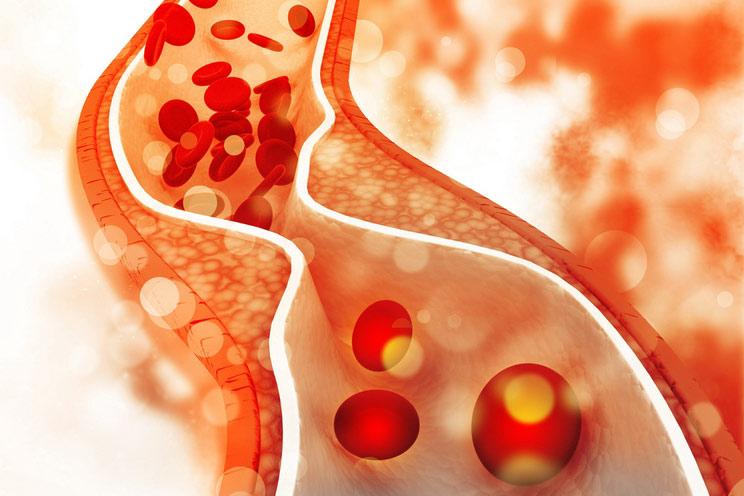
LDL got its bad rap because oxidized LDL can lead to plaque build-up in the arteries. Oxidation happens when inflammation damages cells, and they start functioning abnormally.
Inflammation is the body’s response to injury, but not always in the obvious sense. Injury can happen on the inside of the body as a result of a rogue immune system, poor dietary choices, and chronic conditions.
Doctors use certain blood markers to track inflammation in the body. While genetics can certainly make someone more prone to inflammatory problems, lifestyle factors also have a major role. It’s just that cholesterol is no longer the ultimate problem.
From a dietary standpoint, trans fats and refined sugars ramp up inflammation much faster than foods that contain cholesterol. (6) Unlike cholesterol, which the body produces, trans fats and refined sugars won’t be synthesized in the body if we don’t eat enough. In fact, they aren’t needed at all, and can be quite damaging in a number of ways.
Trans fats are damaged fats that occur as a result of overprocessing foods, and are not the heart-healthy fats that are found in nature. Trans fats are often considered bad because they’re linked with raising “bad” cholesterol, but it isn’t that they raise LDL so much as they damage the existing LDL cells, resulting in plaque deposits that can cause problems. [tweet_quote]LDL got its bad rap because oxidized LDL can lead to plaque build-up in the arteries. Oxidation happens when inflammation damages cells, and they start functioning abnormally.[/tweet_quote]
So how do you know if inflammation is your problem? These two tests should be considered alongside the standard cholesterol and triglycerides measurements to determine actual heart disease or chronic disease risk:
- C-reactive protein test
- Homocysteine test
C-reactive protein measures specific inflammatory markers in the body that can help to determine inflammation levels as well as the potential for narrowing of arteries. While the American Heart Association (which still blames cholesterol for problems) doesn’t think it’s necessary, numerous integrative practitioners use this as a gold standard for determining problematic inflammatory risk. (7)
Homocysteine, a chemical found in the blood, is produced in response to methionine, an amino acid. While everyone needs a certain amount of homocysteine in their blood, elevated levels can be indicative of inflammation and can be irritating for blood vessels, leading to arterial hardening and risk for heart attack. (8) Homocysteine can become elevated in response to poor dietary choices, but it can also be higher in individuals with certain genetic mutations that require harder-to-get nutrients to keep it in check.
Specifically, the genetic mutation called MTHFR indicates difficulty absorbing critical vitamins. When homocysteine is elevated in individuals who have MTHFR mutations, it’s often because they can’t properly metabolize the B vitamins that keep methionine and other body processes in check. To offset this genetic mutation, it is recommended that we limit processed foods and eat a diet rich in high-quality animal products and green vegetables.
4 Ways to Reduce Inflammation with Diet and Lifestyle
Since heart disease is much more complex than just using cholesterol as a scapegoat, understanding the root causes of heart (and most other) disease can lead to an overall preventive lifestyle.
Inflammation is more dangerous to heart health than cholesterol, so it’s important to understand that it can be dramatically impacted with dietary and other lifestyle choices.
1. Eat Anti-Inflammatory Green Vegetables

Green vegetables are rich in folate, antioxidants, and fiber, giving them a trifecta of healthful benefits that not only help to prevent inflammation, but can also help to reverse chronic health problems after they’ve started.
2. Eat More Omega-3 Fatty Acids

Omega-3 fatty acids – like those found in salmon, mackerel, and cod liver oil – differ from other types of fats in that they’re potently anti-inflammatory. Omega-6 fatty acids, commonly found in nuts and seeds, are more pro-inflammatory, but are often eaten in far greater amounts than omega-3s.
Eating omega-3s on a daily basis and limiting intake of omega-6 fatty acids can help to restore balance to this fat ratio, leading to decreased inflammation and improved heart health. (9)
3. Skip Trans Fats, Refined Sugars, and Processed Foods

Trans fats, refined sugars and processed foods can be especially harmful if you have existing inflammatory conditions, known MTHFR mutations, or a family history of heart disease.
Not only do these foods lead to inflammation, they can also wreak havoc on the digestive system as well as contribute to weight problems and hormone imbalance.
4. Manage Stress and Sleep

You can eat all the right foods, exercise, and skip detrimental habits like smoking, but if you’re stressed to the max and sleeping poorly, then you could still have inflammatory markers that are high.
While there is no one-size-fits-all approach to achieving perfect sleep and reduced stress levels, certain habits can contribute to healthy balance:
- Regular exercise
- A bedtime routine
- Reduced smartphone and computer use at night
- Decreased intake of caffeine, alcohol, and other stimulants
- Healthy stress outlets, like therapy or meditation
(Read This Next: Busted – 5 Common Myths About Cholesterol)

 Pork Chops with Apple, Braised Bacon, and Cabbage
Pork Chops with Apple, Braised Bacon, and Cabbage








Show Comments